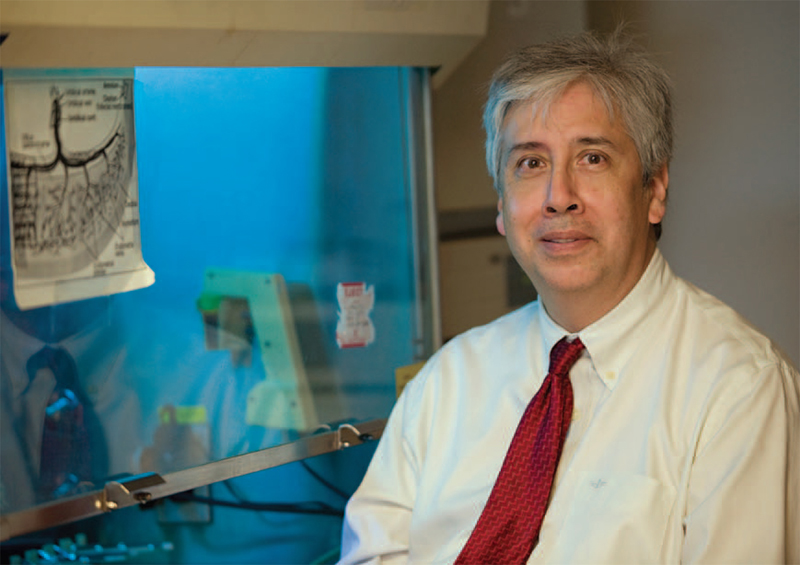
Dr. Alan Moy poses for a photograph at his medical research laboratory in Coralville. A parishioner of St. Mary in Iowa City, Moy adheres to Catholic pro-life values in his cancer research.
For The Catholic Messenger
CORALVILLE — Cellular Engineering Technologies (CET), a biotechnology company, and the John Paul II Medical Research Institute (JP2MRI), a non-profit organization, and the University of Iowa have reached a new milestone in using and creating adult stem cells for research and treatment of disease.
Since 2000, CET and JP2MRI have been focused on creating alternatives to medical research and treatments that use embryonic stem cells. The Catholic Church teaches that each human being is to be respected as a person from the moment of conception and that his or her rights are to be recognized — including at the embryonic stage.
The two Coralville organizations, founded by Dr. Alan Moy, published their research findings in the scientific journal Regenerative Medicine. The study demonstrates a new approach to create induced pluripotent stem cells (iPSC) without the need to use viruses and, more importantly, the standard oncogenes (cancer genes) used to produce iPSC. These are adult stem cells that have been reprogrammed into embryonic-like stem cells.
The study creates new opportunities to extend the diversity and lifelong utility of cord blood. Parents currently bank their child’s cord blood for presumed future private use. However, private cord blood storage has several shortcomings. These include rare and limited therapeutic indications during childhood and an insufficient number and diversity of stem cells to treat chronic disease as children approach adulthood.
The study also reports creation of iPSC from peripheral blood in patients with Cystic Fibrosis and alpha one antitrypsin deficiency, a genetic cause of Chronic Obstructive Pulmonary Disease. Peripheral blood cells are the cellular components of blood, consisting of red blood cells (erythrocytes), white blood cells (leucocytes) and platelets, which are found within the circulating pool of blood and not sequestered in the lymphatic system, spleen, liver or bone marrow.
The production of safer pluripotent stem cells from peripheral blood offer more predictive patient models of disease for drug development without untoward influences from viral and oncogenic effects. Also, the approach provides a safer autologous (patient’s own) pluripotent stem cell therapy for future use. This technology advances personalized and regenerative medicine, drug discovery and bio-banking. Virus-free and oncogene-free iPSC offers broader utility than the direct use of cord blood for a diverse spectrum of diseases that include neurodegenerative, cardiopulmonary, retinal, arthritic, metabolic and autoimmune disorders and cancer.
In response to this scientific breakthrough, JP2MRI and CET are creating a joint venture to establish a commercial, private iPSC bio-bank from a donor’s peripheral blood or samples derived from a donor’s privately banked cord blood. The benefits for the consumer include offering a lifetime personalized iPSC for personalized diagnostics, personalized medicine, more efficient drug development for clinical trials and future autologous stem cell therapies. Individuals can learn more about the private iPSC banking by going to CET’s website (www.celleng-tech.com). For more information, contact: info@celleng-tech.com or phone: (319) 688-7367. Visit the John Paul II Medical Research Institute at www.jp2mri.org.